The Future is Now — Experience It with SPRY at APTA PPS, Booth #807.
Learn More
Stop searching. Start coding smarter with our ICD-10 Lookup Tool.
Try Now
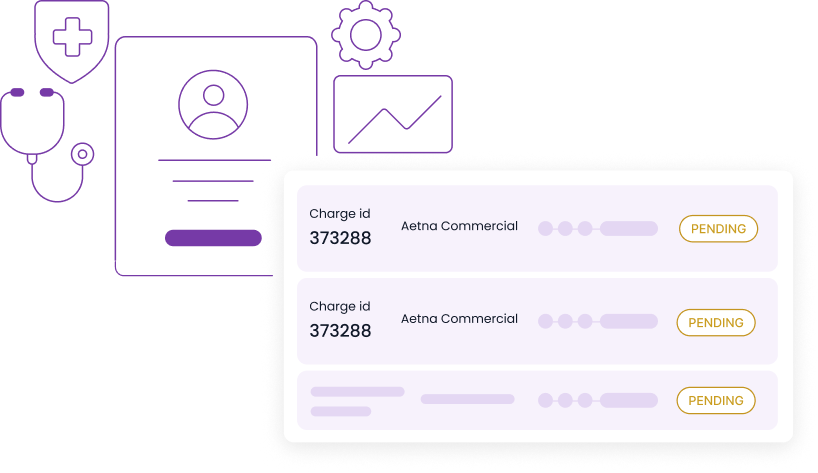
Let SPRY handle billing while you stay on the EMR your team already knows. We take on the complexity, you get back control, cleaner claims, faster payments, and fewer headaches.
Request a Demo




SPRY integrates with your current system so you don’t have to retrain staff or migrate data.
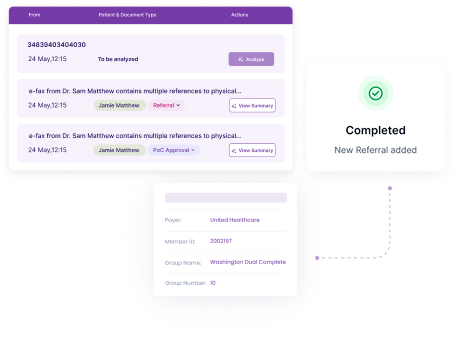

From claim scrubbing to A/R follow-ups, we handle every step while your team continues using the tools they know.
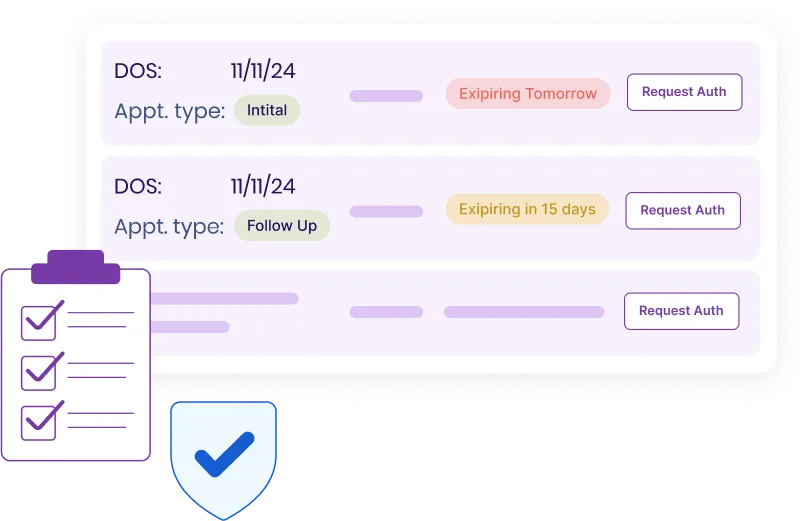
We reduce errors, automate follow-ups, and ensure each claim is coded and submitted with precision.




SPRY provides custom dashboards and weekly updates that keep you informed without overwhelming your team.
Our team handles setup, payer enrollment, and data syncing without burdening your staff or disrupting care delivery.

Your team works with a dedicated RCM partner who understands your EMR, workflows, and business goals.


Need more help? Reach out to us.
SPRY integrates through secure APIs and data bridges that sync patient, charge, and payment information automatically. Your team continues using the same EMR screens, while SPRY works in the background to manage billing and reporting.
We map data directly from your EMR, then apply SPRY’s claim-scrubbing logic before submission. This dual validation catches coding, modifier, and authorization errors early — leading to cleaner claims and faster reimbursements.
Yes. You’ll receive custom dashboards and weekly summaries showing claim status, A/R aging, and collection trends. You get full visibility without needing to log into another system.
No. SPRY adapts to your current workflows and software setup. Your clinicians and front office keep working as usual while our RCM team handles claims, denials, and payments through connected channels.
Our onboarding team builds around your current processes. We handle payer enrollments, credentialing syncs, and data validation while your staff continues normal operations, ensuring zero downtime in patient care.
You’re paired with a dedicated RCM specialist who understands your EMR setup. They communicate directly with your staff for eligibility, authorizations, and follow-ups — no ticket queues, just clear collaboration.