The Future is Now — Experience It with SPRY at APTA PPS, Booth #807.
Learn More
Stop searching. Start coding smarter with our ICD-10 Lookup Tool.
Try Now



.svg)

.svg)



.svg)

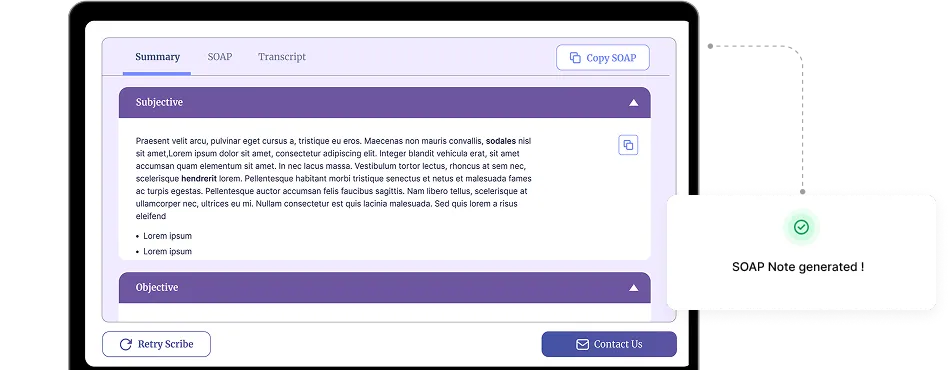
No typing, no hassle—just accurate notes in seconds!







Even experienced rehab therapists can make common errors when writing SOAP notes. These mistakes can affect the quality of patient documentation, lead to miscommunication between care providers, and even cause issues with insurance compliance.
.svg)

.svg)

.svg)

.svg)

.svg)

.svg)

Find answers to the most common questions about Spry Scribe. From features to integration, we've got you covered.
An AI progress note generator is a tool that helps therapists and mental health professionals create accurate and structured progress notes quickly. It uses AI to streamline documentation, ensuring compliance with industry standards like SOAP and DAP formats.
Yes, our AI SOAP note generator is HIPAA-compliant, ensuring the security and confidentiality of patient data. We prioritize privacy and adhere to strict compliance standards for mental health documentation.
An AI therapy note generator analyzes session details and generates comprehensive notes based on SOAP, DAP, or physical Therapy note formats. It saves time and reduces manual effort while improving accuracy.
Yes! We offer a free AI progress note generator to help therapists and healthcare professionals streamline their workflow. You can try it at no cost and upgrade for advanced features.