Webinar: Beyond Fee for Service Direct-to-Employer Care for Clinics Built to Last | Featuring Scott Hebert
Register Now




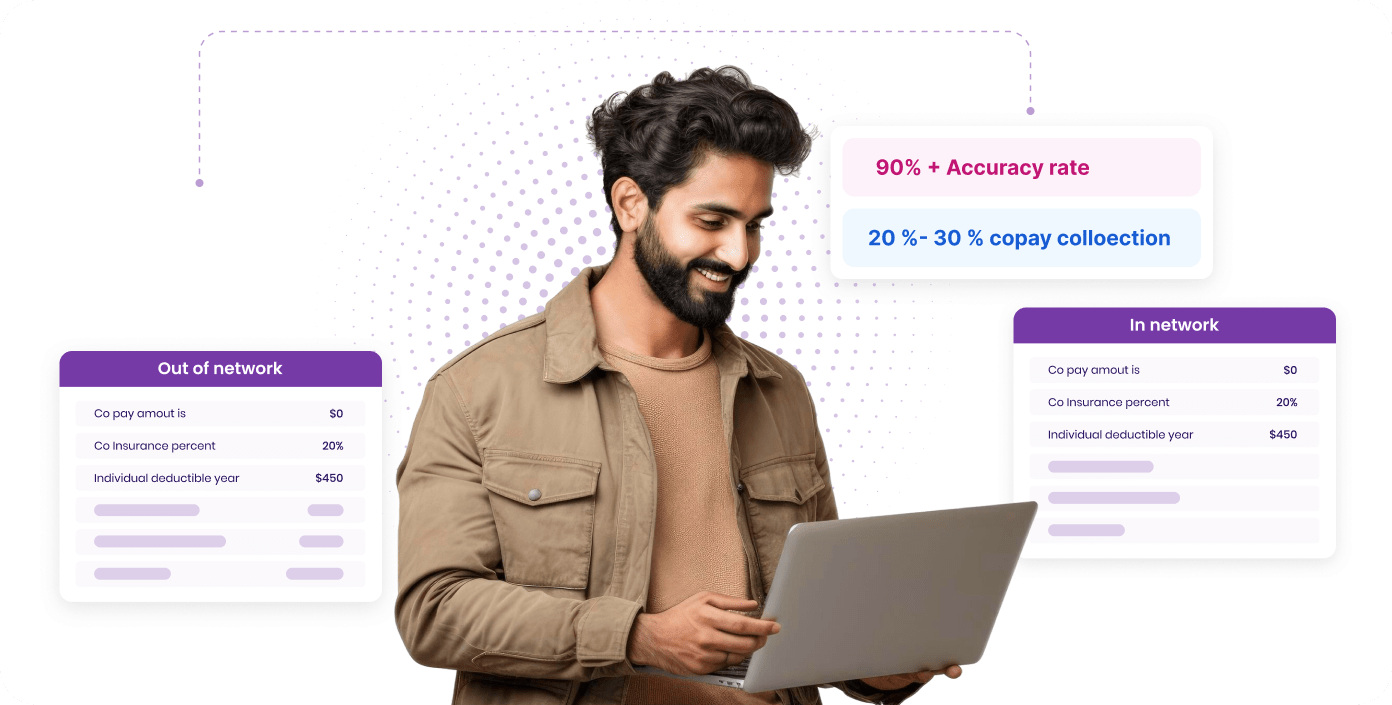
We run eligibility checks so your staff walks in each morning already knowing who’s good to go. No more last-minute scrambling or awkward surprises at check-in.
The right amount is shown at the right time, before the visit even starts. Patients trust the process. Staff has fewer awkward conversations. Balances don’t linger.
Our system flags common coding issues, from missed 8-minute rules to missing modifiers, so billers spend less time fixing, and more time closing the loop.
We route claims according to each payer’s exact needs. Fewer rejections. Less back-and-forth. More peace of mind.
-min.png)
Every denial is tracked. Every one is acted on in 1–2 days. Nothing gets written off without your say-so. You stay in control without needing to micromanage.
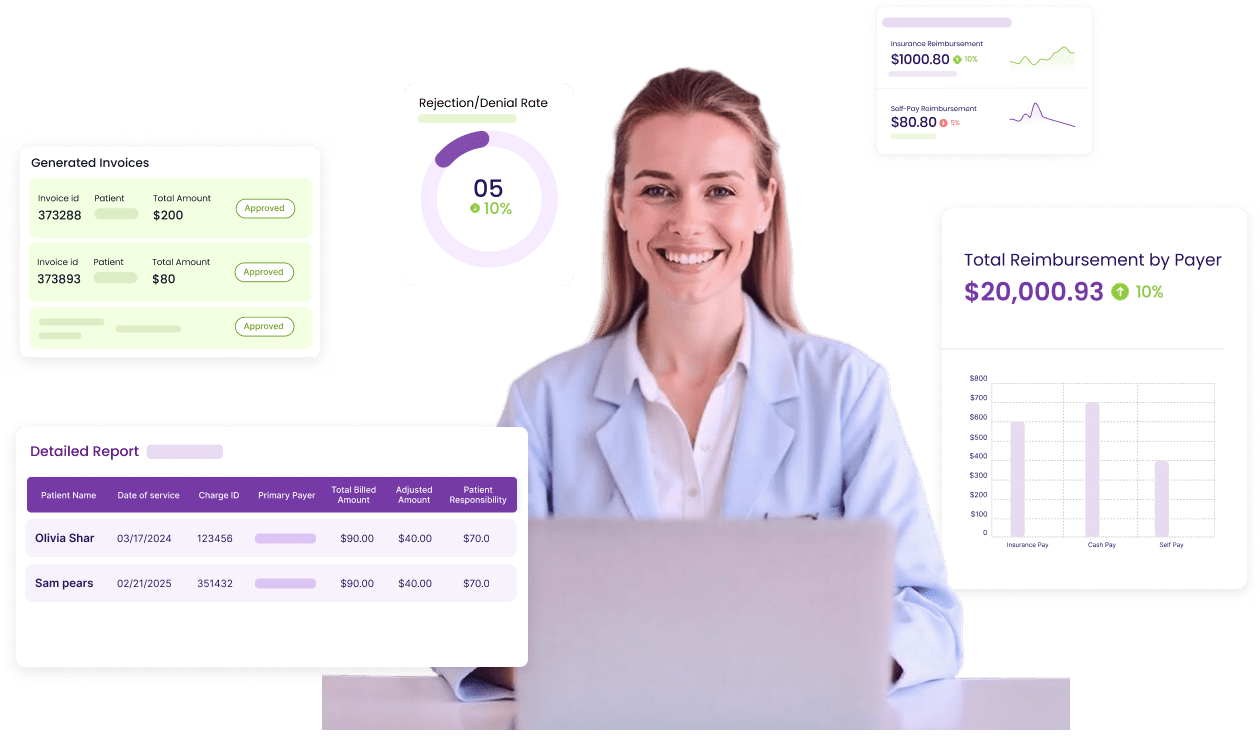
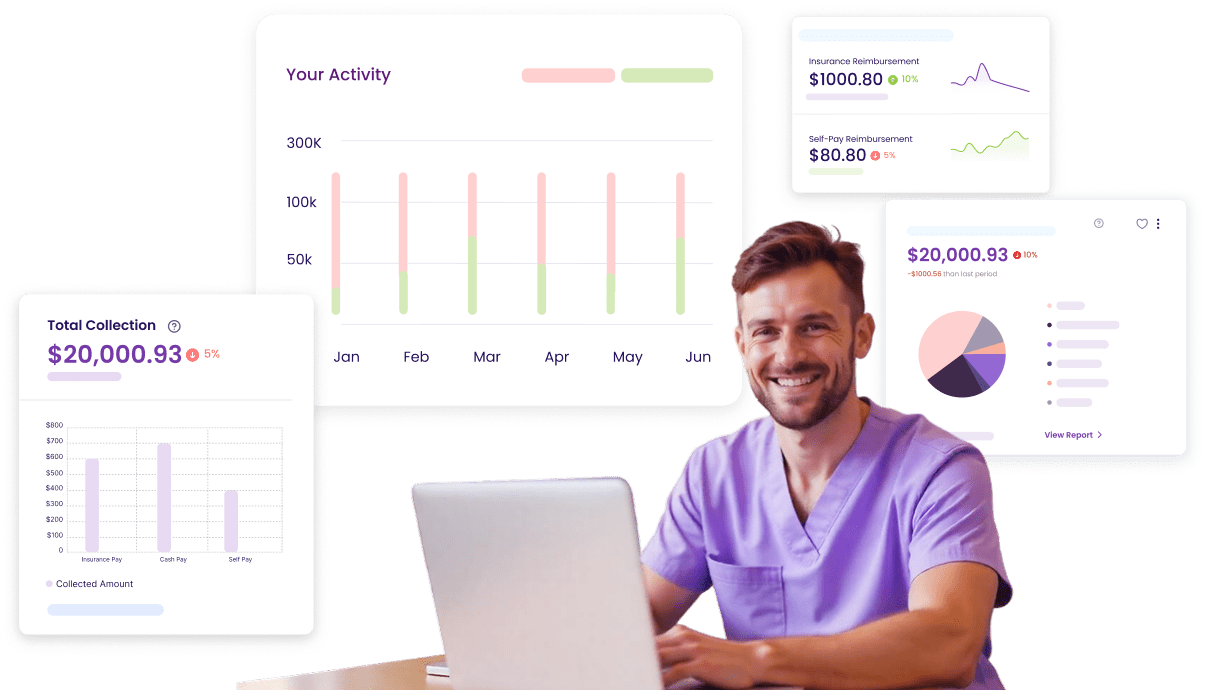
You see what’s clean, what’s delayed, what’s at risk, in one place. No more chasing status updates. No more surprises at month-end.
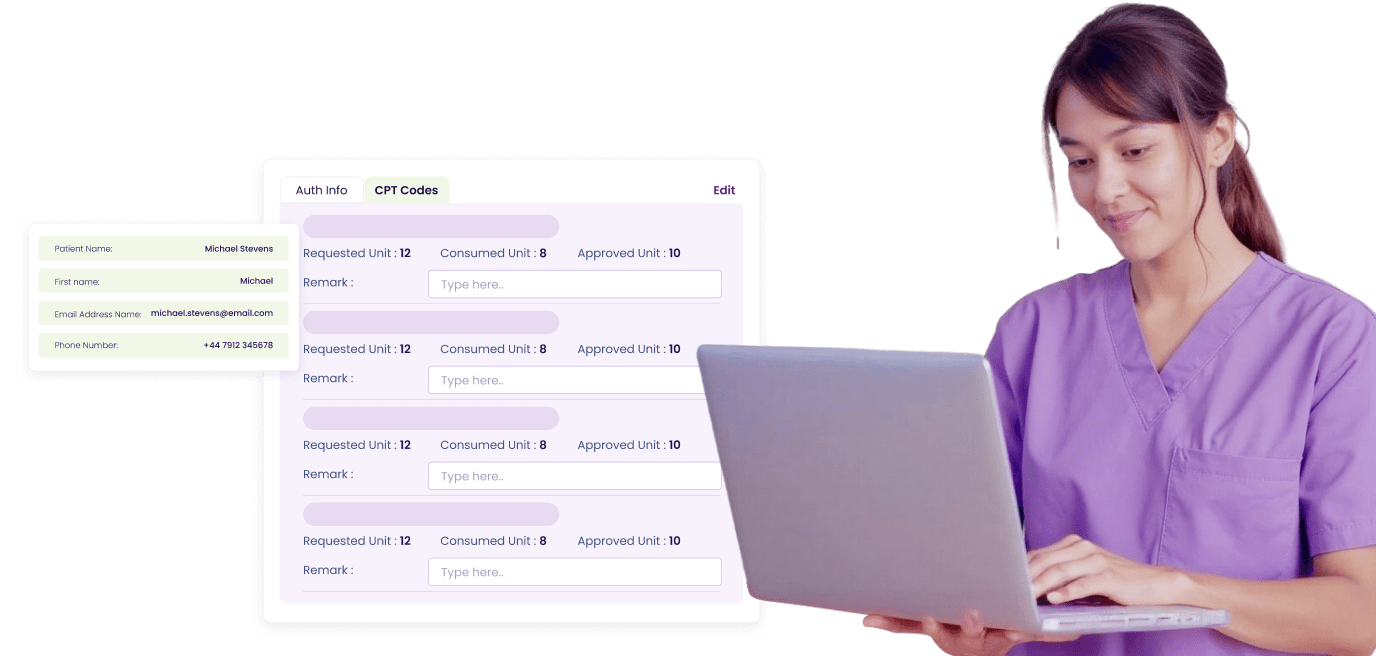
We take care of payer paperwork in the background, tracked, updated, and visible, so you never wonder what’s slowing things down.
-min.png)
Need more help? Reach out to us.
Rejections usually stem from small coding inconsistencies, missing modifiers, incorrect time-based CPT units, or payer-specific format errors. SPRY’s built-in claim scrubber detects these before submission, helping clinics maintain over 95% clean claims on the first pass.
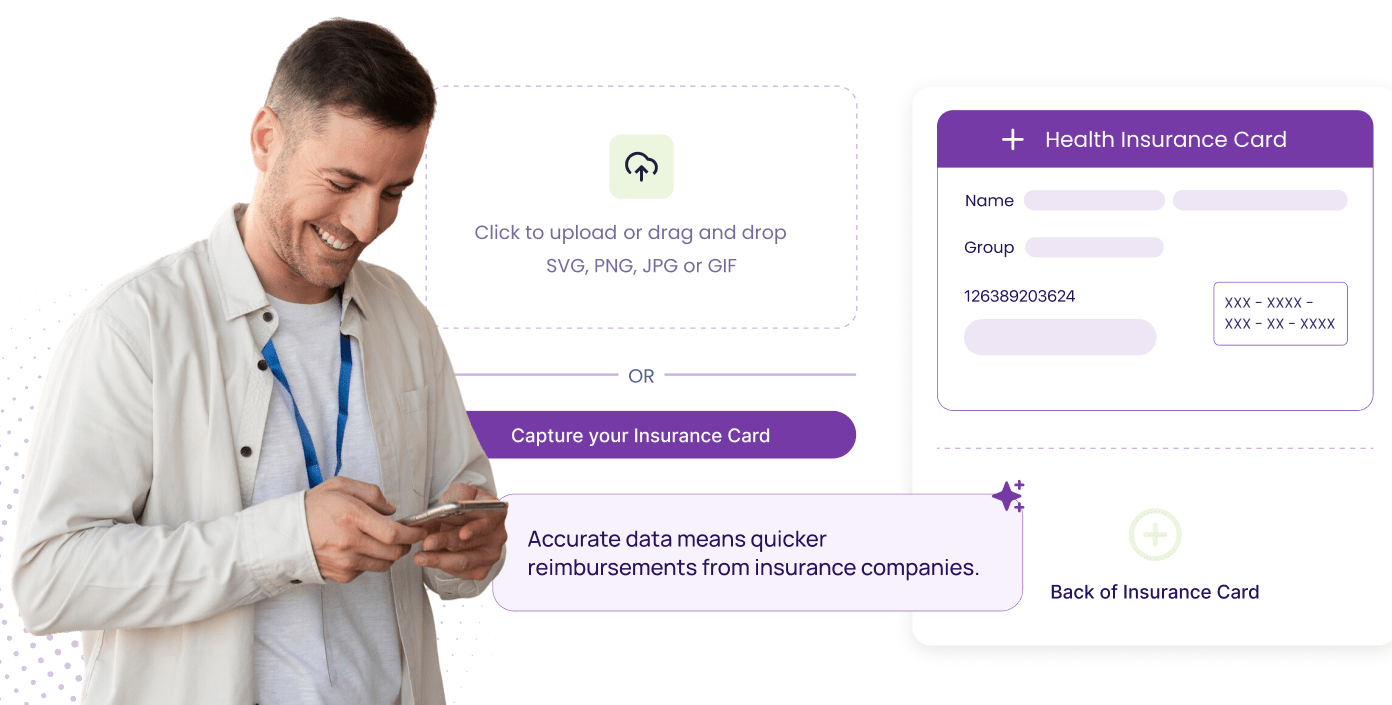
SPRY runs daily eligibility checks for upcoming visits. If a plan or deductible changes, staff are alerted before the appointment, so copays and authorizations stay accurate and care never gets delayed.
Yes. SPRY’s RCM dashboard updates continuously, showing what’s paid, pending, or at risk. You can spot bottlenecks early, review payer trends, and close out month-end faster with zero guesswork.
Every denial is automatically logged, assigned, and worked within 24–48 hours. You can view resolution notes directly in the dashboard, ensuring accountability without manual follow-up or long email trails.
SPRY’s compliance engine cross-references each note against payer rules and therapy coding standards. It flags incomplete or conflicting entries instantly, so billers can correct them before claims are submitted.
All credentialing and enrollment requests are tracked inside SPRY with live status updates. You can see exactly which applications are pending, which payers are waiting on documents, and when approvals clear — no more waiting for updates by email..