The Future is Now — Experience It with SPRY at APTA PPS, Booth #807.
Learn More
Stop searching. Start coding smarter with our ICD-10 Lookup Tool.
Try Now





Industry-first automation that eliminates manual tasks, reduces errors, and saves time.
Automatic KX modifier appending ensures seamless Medicare Part-B compliance before claim submission.
.webp)
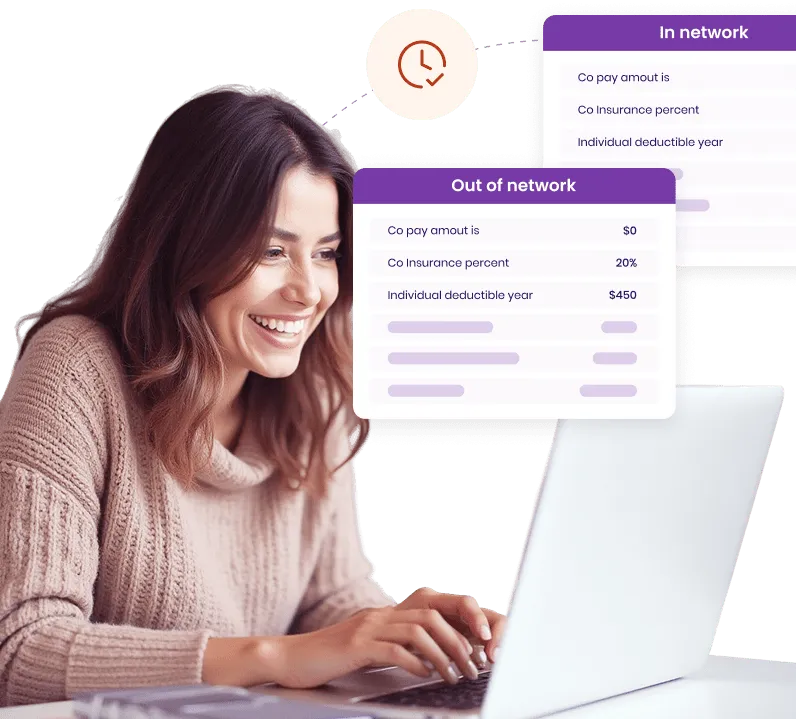
Instant, accurate results with no back-and-forth.
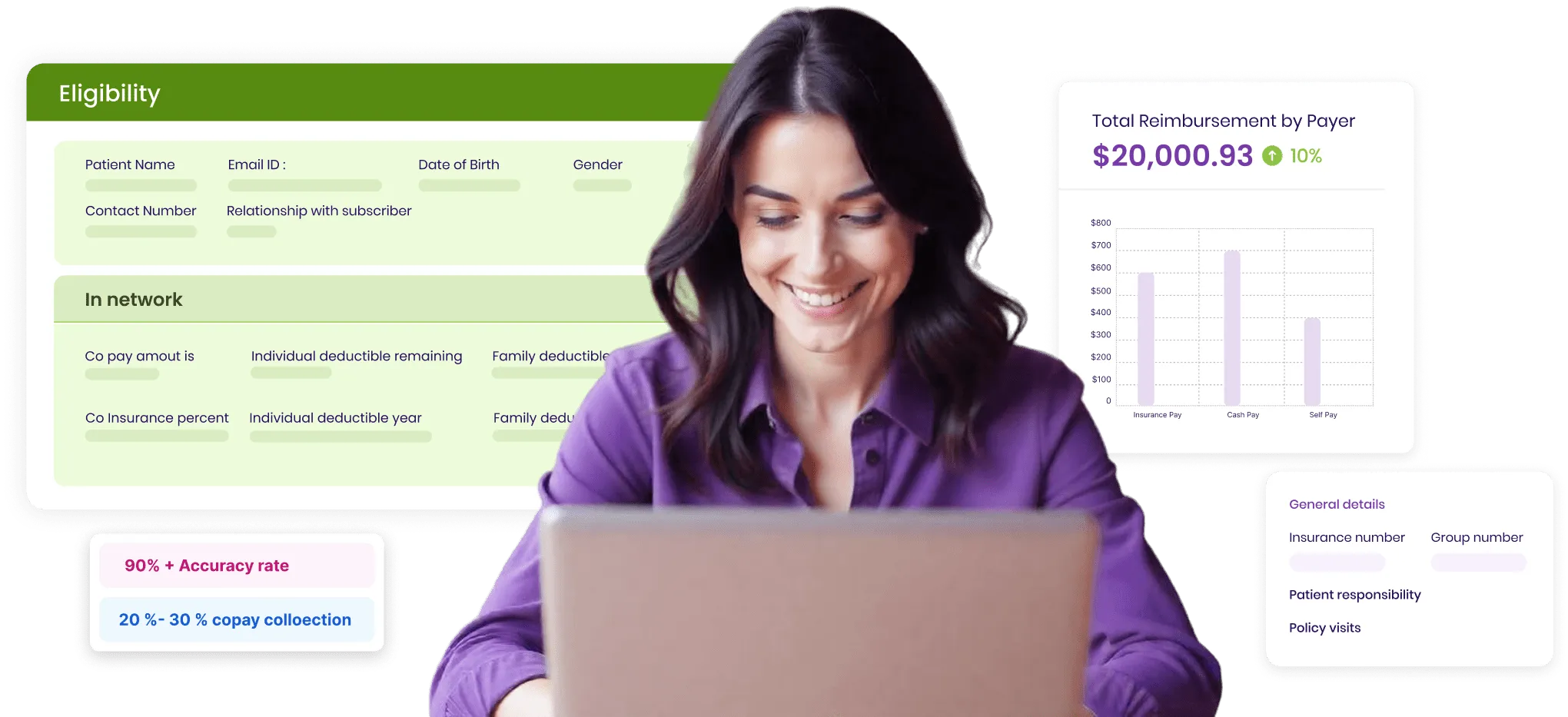
95%+ accuracy rate ensures correct coverage details, leading to 20-30% higher copay collections.
.webp)
Fits effortlessly into your existing workflow.
.webp)
Simple, intuitive, and built for speed.
.webp)
Fewer denials, faster reimbursements, and higher upfront payments drive better cash flow.
.webp)
Automated verification eliminates manual calls, reduces admin workload by 60%, and speeds up patient intake.
Need more help? Reach out to us.
SPRY works with on- and off-exchange insurance providers, Medicare, and workers' compensation plans.
Yes! By verifying insurance details upfront, SPRY reduces rejections and unexpected costs for patients, improving claim approval rates.
SPRY offers seamless integration with its built-in billing system and EMR, streamlining workflow and eliminating duplicate data entry.
SPRY pulls real-time eligibility data integrated directly with your billing system, minimizing errors from manual entry and ensuring up-to-date information.
Yes, it’s a fully automated system with a single-tap eligibility check, removing the need for time-consuming phone calls.
Eligibility verification is nearly instant, giving you access to critical patient coverage information in seconds.