Summary: This comprehensive comparison of SOAP and DAP notes highlights their distinct structures and applications in clinical documentation. SOAP notes, with their four-part format, are ideal for complex cases requiring detailed information, while DAP notes offer a simpler three-section approach suitable for standard follow-ups. Understanding these differences can enhance documentation efficiency, allowing healthcare professionals to focus more on patient care. For those seeking an all-in-one solution to streamline their documentation processes, SPRY is the top choice, offering proven efficiency gains over traditional methods.
Introduction
Clinical documentation takes valuable time away from patient care each day. Selecting between SOAP and DAP notes formats directly affects your documentation efficiency and overall care quality.
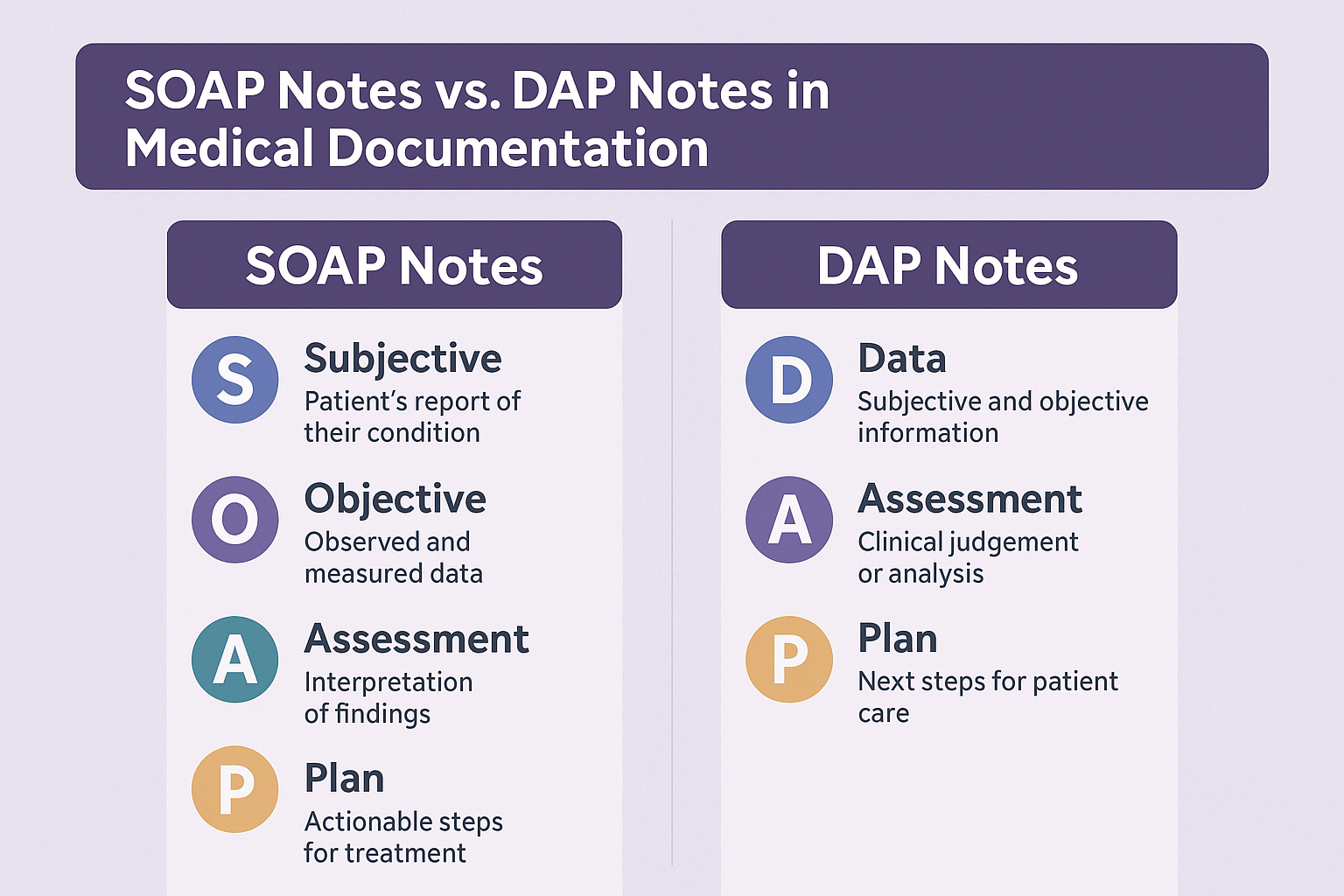
SOAP notes feature a four-part structure perfect for complex cases requiring detailed information capture. The format supports thorough assessment and treatment planning across multiple healthcare disciplines. DAP notes provide a more concise three-section approach ideal for standard follow-up visits where simplicity matters most.
This comparison examines both documentation methods side-by-side, highlighting their structures, practical applications, and key benefits. Understanding which format suits specific clinical scenarios helps you implement the right approach for your practice needs. Making this choice wisely means less time writing notes and more time focusing on patient care.
The Evolution of Clinical Documentation
Clinical documentation history spans thousands of years, beginning with ancient Egyptian medical records around 1550 BCE. These early records served primarily as teaching tools for future physicians, documenting treatments and observations for educational purposes.
Origins of Structured Progress Notes in Healthcare
Hippocrates (460-370 BCE) established early documentation foundations through medical texts containing physician recommendations, procedure descriptions, and prescriptions. Arabic physicians later expanded these practices with more detailed medical records.
Structured documentation took a major step forward in the late 19th century when hospitals implemented standardized forms to organize the previously free-form physician notes. This standardization improved medical record analysis but created initial resistance among doctors who felt they lost narrative depth in their documentation.
The documentation landscape changed dramatically in 1971 when Dr. Lawrence Weed developed the Problem-Oriented Medical Record (POMR), addressing the lack of standardized processes. SOAP notes emerged from this framework, fundamentally changing how clinicians recorded patient information.
How Documentation Standards Have Changed Over Time
Medical records evolved beyond basic patient care throughout the 20th century. Records became legal documents with specific retention requirements, educational tools, and defined work products for physician payment.
Electronic health records emerged and grew rapidly starting in the 1960s using punch cards. The HITECH Act later provided significant incentives for EHR adoption, transforming documentation practices across healthcare settings.
Current documentation standards continue evolving under regulations like the 21st Century Cures Act, which prioritizes interoperability and patient record access. CMS modified outpatient evaluation requirements in 2021, removing certain documentation elements to reduce administrative burden.
Despite ongoing changes, documentation's core purpose remains consistent: tracking patient conditions and communicating clinical reasoning to the care team – with additional stakeholder requirements added through the decades.
Understanding SOAP Notes: Structure and Purpose
SOAP notes function as the foundation of structured clinical documentation across healthcare disciplines. Dr. Lawrence Weed developed these notes in the 1960s as part of the problem-oriented medical record (POMR) system. These standardized notes now play an essential role in documenting patient encounters.
What Does SOAP Stand for in Clinical Documentation?
SOAP represents four core components that create comprehensive clinical documentation:
- S (Subjective): Records the patient's self-reported symptoms, concerns, and experiences using their own words
- O (Objective): Documents measurable, observable data including vital signs, physical examination findings, and test results
- A (Assessment): Presents the clinician's analysis, diagnosis, and professional evaluation based on subjective and objective information
- P (Plan): Details the proposed treatment approach, future session goals, and next steps for patient care
This structured approach guides clinicians through systematic patient evaluation, ensuring thorough documentation across all healthcare settings.
Key Components of Effective SOAP Notes
Quality SOAP notes share several important characteristics. They capture relevant details without adding unnecessary information. The subjective section must include the patient's chief complaint using their exact words whenever possible.
The objective section requires quantifiable information anyone observing the interaction could verify. Clinician assessment should present professional judgment based solely on verifiable evidence. The plan section must outline specific interventions, treatment frequency, and expected outcomes.
Benefits of Using SOAP Notes in Therapy Sessions
Therapy settings gain numerous advantages from SOAP notes. They establish a universal system for recording treatment details and benchmarks, facilitating communication between providers. This standardization helps identify patterns and evaluate treatment effectiveness over time.
SOAP notes help clinicians track client progress, maintain organization, and share information with insurance companies and other healthcare providers. They serve as valuable legal documentation, protecting practices during disputes or insurance claims.
SOAP notes streamline clinical workflows through a clear, standardized format that enhances decision-making while keeping important details readily accessible – supporting better patient care through consistent documentation.
Exploring DAP Notes: Format and Applications
DAP notes offer a streamlined approach to clinical documentation, particularly popular among mental health professionals due to their clarity and efficiency. Unlike more complex methods, DAP notes deliver a straightforward yet thorough framework for documenting client interactions.
What Does DAP Stand for in Progress Notes?
DAP represents Data, Assessment, and Plan, creating a logical documentation flow for clinicians. This three-part structure emerged in the 1980s as a simplified alternative to other documentation formats, designed to balance thoroughness with efficiency. Some clinicians expand this format to DARP by adding a "Response" section, especially when tracking client reactions to specific interventions. DAP notes provide clinicians a clear structure to reflect on client progress in an organized manner.
Essential Elements of Comprehensive DAP Documentation
Each DAP component serves distinct purposes:
Data section captures observable information without interpretation. This includes client statements, reported symptoms, mental status, screening results, and applied interventions. Clinicians record factual information, often using direct client quotes, combining both subjective and objective observations.
Assessment section allows clinicians to apply professional judgment when interpreting collected data. This typically includes progress evaluation, diagnosis updates, self-harm or suicide risk assessments, and how client status relates to treatment goals. This section specifically reflects the clinician's analysis based on collected data.
Plan section outlines future treatment steps, including next session scheduling, homework assignments, referrals, consultation plans, and treatment plan modifications. This creates a roadmap for future sessions directly responding to the assessment.
When Do DAP Notes Work Best for Physical Therapists?
DAP notes excel in specific clinical scenarios. They perform best in brief, focused sessions where capturing essential information without unnecessary complexity matters most. They help track incremental progress across standard sessions. During high-stress situations, DAP notes enable quick documentation prioritizing actionable steps.
Physical therapists often prefer DAP notes because they remove the need to distinguish between subjective and objective input—everything is simply recorded as "data." This streamlined structure allows for quicker documentation, making it a great choice for busy PTs who want to maintain thorough records without slowing down their workflow.
SOAP vs DAP Notes: Key Differences and Similarities
Practice requirements determine your choice between SOAP and DAP notes. While both formats serve identical documentation purposes, they differ substantially in structure, approach, and time efficiency. Understanding these differences helps select the format best suited for your clinical workflow.
Structure Comparison: 4-part vs 3-part Format
SOAP notes utilize a four-section structure: Subjective, Objective, Assessment, and Plan. DAP notes feature a more condensed three-section approach: Data, Assessment, and Plan. This fundamental difference directly impacts information organization throughout the documentation process.
SOAP notes assign each component a distinct purpose with clear boundaries. This separation creates a highly structured record guiding clinicians through methodical assessment and planning. DAP notes combine what would be separate Subjective and Objective sections into a single Data section, creating a more streamlined documentation experience.
Documentation Approach: Separated vs Combined Observations
SOAP notes deliberately separate patient-reported information from clinician observations. This distinction proves particularly valuable in medical or multidisciplinary settings where differentiating between patient experiences and measurable clinical findings matters significantly.
DAP notes combine all session information—both client-reported and clinician-observed—into one Data section. Therapists often prefer this approach because it better accommodates behavioral health assessments where the line between subjective experiences and objective observations frequently blurs.
Time Efficiency: Which Format Streamlines Your Workflow?
DAP notes generally offer time efficiency advantages. By combining subjective and objective information under one heading, they typically require less completion time than SOAP notes. This streamlined approach saves valuable minutes, especially during routine follow-ups or straightforward cases.
SOAP notes excel when detailed clinical reasoning and comprehensive documentation become necessary. Their structured format supports thorough assessment and treatment planning for complex cases, initial evaluations, or situations requiring clear communication between multiple providers.
Both formats satisfy insurance requirements when properly implemented. Your selection should match your practice setting, documentation needs, and personal preferences for organizing clinical information.
Comparison Table
Choosing the Right Format for Your Practice
Documentation format selection demands careful evaluation of your clinical environment. The difference between SOAP and DAP notes becomes crucial when aligning your documentation approach with practice requirements.
Practice Setting Considerations
Practice environment directly determines which documentation format suits your needs best. SOAP notes perform exceptionally well in multidisciplinary settings where detailed documentation facilitates communication between diverse providers. These structured notes originated in medical contexts, making them familiar to physicians, nurses, and other healthcare professionals.
DAP notes show particular strength in mental health practices where subjective and objective information boundaries frequently overlap. Behavioral health practitioners typically work with limited objective information, making the "O" in SOAP potentially confusing or difficult to complete. Many therapists, therefore, prefer DAP's integrated approach for counseling sessions.
Client Complexity and Documentation Needs
Case complexity should guide format selection. Initial evaluations, lengthy visits, and complex cases requiring comprehensive documentation benefit from SOAP notes' detailed structure. Their four-part format supports thorough clinical reasoning and helps justify insurance billing for complex interventions.
Follow-up appointments, routine therapy sessions, and brief interventions typically work better with DAP notes. This streamlined approach eliminates redundancy while capturing essential information, saving valuable time during busy clinical days.
Insurance and Compliance Requirements
Documentation must meet regulatory and insurance requirements regardless of format choice. From a legal perspective, either format satisfies requirements when sessions are documented appropriately. Insurance companies maintain specific expectations:
- Notes must be completed and signed within 72 hours of each session (48 hours for Medicare/Medicaid)
- Documentation must justify medical necessity for services provided
- Records must include sufficient detail supporting the billed care level
While SOAP notes originated in medical settings, both formats satisfy insurance requirements when properly executed. Some payers, accrediting bodies, and regulators may impose more specific requirements affecting your documentation choices.
Templates and Examples for Effective Documentation
Well-designed templates save precious time for clinicians dealing with documentation requirements. These ready-made frameworks allow greater focus on patient care while maintaining complete records.
SOAP Notes Template With Practical Examples
SOAP templates offer a structured four-part framework guiding thorough documentation:
Subjective (S): Record the client's reported experiences, feelings, and concerns. Example: "Client reported feeling 'stressed out' and 'overwhelmed.' Stated, 'I've been worrying constantly and can't relax.' Reports trouble sleeping for the past week."
Objective (O): Note observable, measurable data. Example: "Client exhibited signs of anxiety, including rapid speech, leg shaking, and difficulty maintaining eye contact. Apologized frequently for 'rambling.'"
Assessment (A): Combine subjective and objective evidence for diagnosis. Example: "Anxiety. Insomnia related to excessive worrying/stress."
Plan (P): Specify next actions. Example: "Discussed relaxation techniques. Recommended limiting screen time before bed. Follow up in two weeks."
DAP Notes Template With Real-World Applications
DAP templates merge subjective and objective elements for efficient documentation:
Data (D): Capture all session information. Example: "Client reported on time for third session. Well-groomed and oriented. Reports feeling 'a little bit better' since last session. BDI-II score: 14 (moderate range)."
Assessment (A): Offer clinical interpretation. Example: "Reported reduced sleep symptoms, improved mood, and better BDI-II score suggest progress toward reducing depressive symptoms below diagnostic threshold."
Plan (P): Outline next steps. Example: "Next session scheduled Thursday at 10:00 am. Assigned thought record chart. Provided financial advisor referrals."
Tips for Customizing Templates to Your Specific Needs
Schedule regular documentation time rather than catching up evenings or weekends to effectively implement templates. Some clinicians prefer rearranging components—using APSO order instead of traditional SOAP format.
SOAP notes typically serve complex cases requiring detailed documentation best, while DAP notes work more efficiently for follow-up visits or straightforward sessions.
Implementing Documentation Best Practices
Quality documentation goes beyond selecting appropriate formats—it requires consistent application of best practices. Effective use of SOAP notes and DAP notes depends on developing habits balancing efficiency with thoroughness.
Time-Saving Documentation Strategies
Complete documentation promptly after sessions, preferably within 24-48 hours to maintain accuracy and demonstrate professionalism. This timely approach affects patient care quality directly, not just regulatory compliance. Outpatient therapy progress notes typically range from 100-300 words, balancing detail with brevity.
Efficiency improvements include:
- Documenting during or immediately following sessions
- Using consistent templates matching your preferred format
- Setting aside dedicated documentation blocks in your schedule
Modifying exam room layout to maintain patient eye contact while documenting significantly improves workflow. Strong typing skills eliminate post-session dictation needs.
Ensuring Compliance While Maintaining Clinical Focus
Proper documentation fulfills both clinical needs and regulatory requirements simultaneously. Clinical Documentation Integrity (CDI) programs assist providers in capturing patient information accurately without compromising care quality. The American Health Information Management Association states documentation must "facilitate accurate, complete, and consistent clinical documentation".
Notes function as official medical records potentially viewed by other clinicians or referenced in legal proceedings. Insurance providers typically require note completion within 72 hours (48 hours for Medicare/Medicaid).
Digital Tools and Templates for Modern Practices
EHR systems offer customizable templates supporting both SOAP and DAP formats. These digital tools enhance documentation by auto-filling recurring information, reducing errors while improving consistency.
AI-powered documentation assistants like SPRY's AI Scribe now generate comprehensive progress notes from brief session summaries. These solutions automatically integrate treatment plan goals and evidence-based practices, cutting documentation time from 5-10 minutes per session to just 30-60 seconds.
Conclusion
SOAP and DAP notes both fulfill essential clinical documentation purposes, each performing best in specific scenarios. SOAP notes deliver superior results when detailed, structured documentation matters most - particularly for complex cases needing extensive clinical reasoning or multidisciplinary communication. DAP notes show their value during routine follow-ups and therapy sessions where documentation efficiency becomes the priority.
Your practice needs, client complexity, and documentation requirements should guide format selection. SOAP notes provide comprehensive structure through their four-part organization, while DAP notes offer a simplified yet thorough approach many mental health professionals find more practical.
Whichever format you select, consistent documentation practices remain essential for quality patient care and regulatory compliance. Effective clinical documentation doesn't require choosing the "better" format but selecting the approach supporting your practice goals while upholding quality patient care standards. Whether using SOAP or DAP notes, focus on delivering quality care while creating clear, compliant documentation that serves your clinical needs.
FAQs
Q1. What are the main differences between SOAP and DAP notes?
SOAP notes use a four-part structure (Subjective, Objective, Assessment, Plan), while DAP notes use a three-part structure (Data, Assessment, Plan). SOAP notes separate patient-reported information from clinician observations, whereas DAP notes combine all session information into a single Data section. SOAP notes are typically more detailed and suited for complex cases, while DAP notes are more streamlined and efficient for routine visits.
Q2. When should I use SOAP notes versus DAP notes?
Use SOAP notes for complex cases, initial evaluations, or in multidisciplinary settings where detailed documentation is crucial. DAP notes are better suited for routine follow-ups, brief interventions, and mental health practices where quick, focused documentation is needed.
Q3. Are SOAP notes still relevant in modern healthcare?
Yes, SOAP notes remain highly relevant. While they originated in the 1970s, they continue to be widely used across healthcare disciplines. Their structured format supports thorough assessment, treatment planning, and clear communication between providers, making them valuable in many clinical settings.
Q4. How do SOAP and DAP notes compare in terms of time efficiency?
DAP notes are generally faster to complete due to their streamlined approach, combining subjective and objective information into one section. SOAP notes, while more time-consuming, provide a more detailed structure that supports comprehensive documentation for complex cases.
Q5. Can both SOAP and DAP notes meet insurance and compliance requirements?
Yes, both SOAP and DAP notes can satisfy insurance and compliance requirements when properly executed. The key is to ensure that your documentation, regardless of format, includes sufficient detail to justify medical necessity, supports the level of care billed, and is completed within the required timeframe (typically 48-72 hours after a session).
Reduce costs and improve your reimbursement rate with a modern, all-in-one clinic management software.
Get a DemoLegal Disclosure:- Comparative information presented reflects our records as of Nov 2025. Product features, pricing, and availability for both our products and competitors' offerings may change over time. Statements about competitors are based on publicly available information, market research, and customer feedback; supporting documentation and sources are available upon request. Performance metrics and customer outcomes represent reported experiences that may vary based on facility configuration, existing workflows, staff adoption, and payer mix. We recommend conducting your own due diligence and verifying current features, pricing, and capabilities directly with each vendor when making software evaluation decisions. This content is for informational purposes only and does not constitute legal, financial, or business advice.










